After a break due to various reasons, back at writing something. So, recently I had an opportunity to participate in a project on Low Back Pain (LBP). Participating in the project led to a lot of reading, which to my surprise, rather than clearing my doubts, created more doubts. There is so much ambiguity present in terminology and diagnostic labels that it leads to confusion. Secondly, the research on LBP is immense. There is a wide variety of papers, with some focusing on biopsychosocial models, beliefs, and impact of LBP while others focused on the treatment and more mechanical aspects of LBP. This blog is just an attempt for me to clear my head and organize the concepts somehow!
We know that LBP is a symptom and not a disease. Back pain, like other musculoskeletal pains, can be a resultant of multiple factors. So, this present blog will focus on the factors and causes that may contribute to LBP.
The best approach to identify the cause is to explain them within a biopsychosocial (BPS) framework. The BPS model is an interdisciplinary model that looks at the interconnection between biology, psychology, and socio-environmental factors.
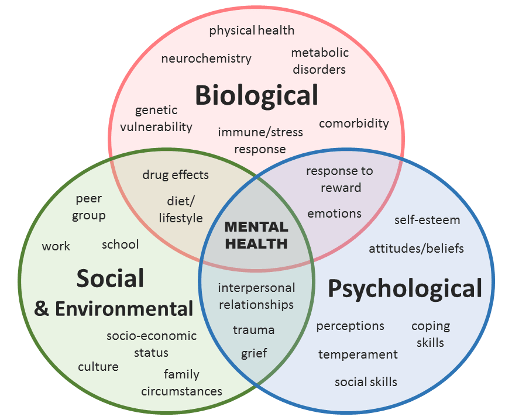
Generally, there is a lot of confusion regarding the word “biopsychosocial”; clinicians frequently assume that the BPS model’s three elements are separate drivers of pain and health, which is not plausible. I would recommend you read the blog “What’s in a word? It’s all Biopsychosocial, and a part of the complex human “ecosystem” by David Poulter.
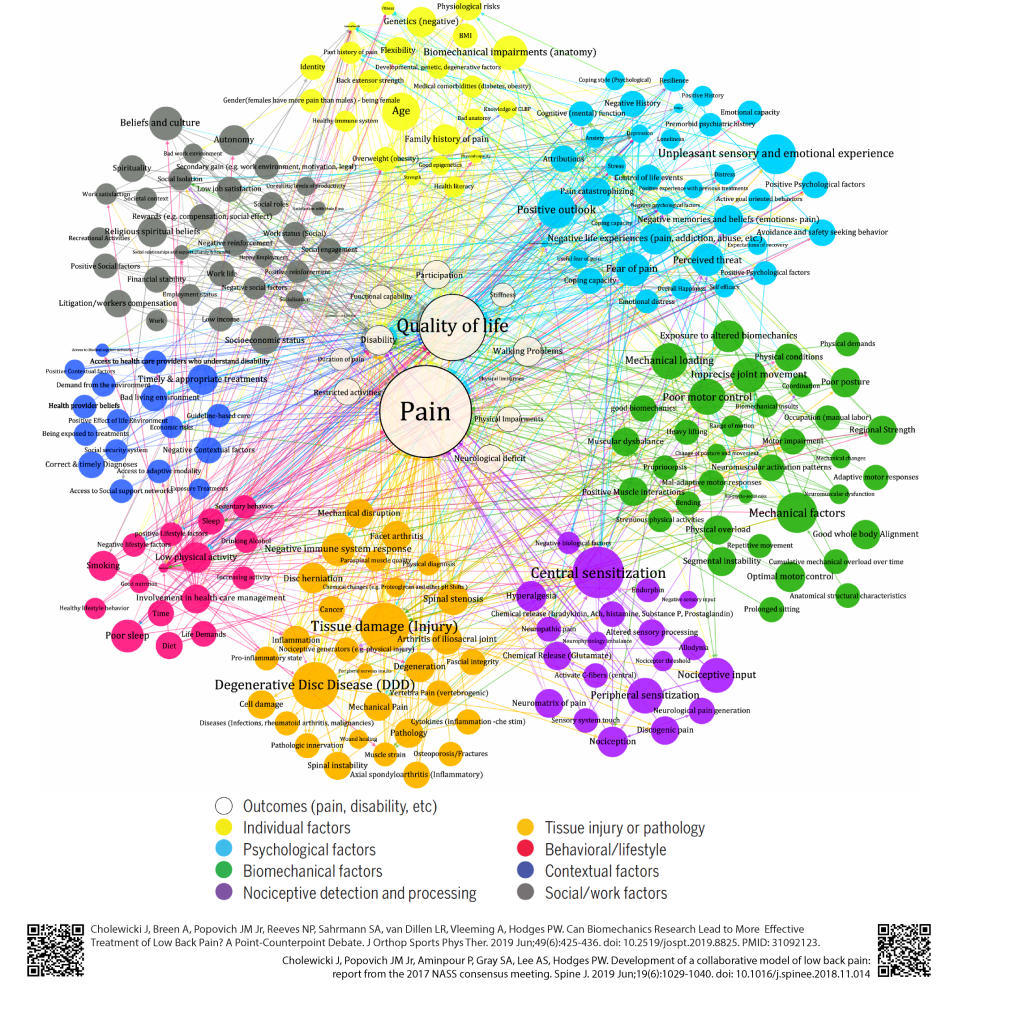
In terms of factors contributing to LBP, a recent paper published in JOSPT by Jacek Cholewicki et al. talks about the different factors (color circles) contributing to low back pain. The image below taken from the article reflects that LBP is complex and multi-factorial. It’s essential that while assessing an individual having LBP, we must look at the big picture.
Moreover, there have been studies that attribute LBP to a pathoanatomic cause. That means there is an underlying tissue that is the source of pain. Although this has been the conventional method of understanding LBP, recent studies do not support this notion. A recent study published in the Spine journal “Association of Lumbar MRI Findings with Current and Future Back Pain in a Population-Based Cohort” demonstrated that degenerative findings on the MRI do not have clinically important associations with LBP.
Similarly, a widely cited study by Brinjikji and colleagues concluded that, “Imaging findings of spine degeneration are present in high proportions of asymptomatic individuals, increasing with age. Many imaging-based degenerative features are likely part of normal aging and un-associated with pain. These imaging findings must be interpreted in the context of the patient’s clinical condition”.

These studies and many other similar ones must make a clinician reflect on the factors and causes that contribute to LBP. Scan findings must always be evaluated along with the patient’s history and clinical examination.
I would also like to highlight a study by Ganesan et al. published in the Asian Journal of Spine. They explored the risk factors for Low Back Pain in 1,355 Young Indian Adults. Their results indicated that the following factors were associated with LBP in young adults: marital status, previous history of spine problems, strenuous exercise, job satisfaction, monotony, stress, the daily number of studying hours, and family history of spine problems. However, age, sex, smoking, alcoholism, coffee intake, mode and duration of travel, diet, frequency of weightlifting, wearing heels, studying posture, and frequency and type of sports activities were not associated with LBP.
Overall, the evidence stresses the need for a biopsychosocial framework to understand the causes and risk factors contributing to LBP.

So, I would like to infer that it’s important to understand the person in front of us that is experiencing and reporting pain. The causes are diverse and must be explored in a biopsychosocial framework.
Hope you enjoyed the blog, I would love to know your thoughts on this.
Ammar Suhail PT
References (All the links are working in the text)
Cholewicki J, Breen A, Popovich Jr JM, Reeves NP, Sahrmann SA, Van Dillen LR, Vleeming A, Hodges PW. Can biomechanics research lead to more effective treatment of low back pain? A point-counterpoint debate. journal of orthopaedic & sports physical therapy. 2019 Jun;49(6):425-36.
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, Halabi S, Turner JA, Avins AL, James K, Wald JT. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. American Journal of Neuroradiology. 2015 Apr 1;36(4):811-6.
Kasch R, Truthmann J, Hancock MJ, Maher CG, Otto M, Nell C, Reichwein N, Bülow R, Chenot JF, Hofer A, Wassilew G. Association of Lumbar MRI Findings with Current and Future Back Pain in a Population-Based Cohort Study. Spine. 2021 Aug 18.
Ganesan S, Acharya AS, Chauhan R, Acharya S. Prevalence and risk factors for low back pain in 1,355 young adults: a cross-sectional study. Asian spine journal. 2017 Aug;11(4):610.
Leave a comment