Hello everyone!
If you’ve ever wondered why your doctor, teacher, or social worker suddenly started quoting “the latest research” before making a decision, you’re brushing up against something called evidence-based practice (EBP). It sounds formal, maybe even a bit intimidating, but at its heart, it’s just a disciplined way of saying: Let’s use what actually works, not just what feels right. Let’s walk through where this idea came from, what it really means, and why it matters without the jargon overload.
A Brief History: From EBM to EBP
The roots of Evidence-Based Medicine (EBM) can be traced back to the early 1990s, largely attributed to the work of Gordon Guyatt and colleagues at McMaster University. Guyatt first introduced the term “EBM” in 1991 as a new way of teaching and practicing clinical medicine built on rigorous appraisal of research evidence rather than tradition or expert opinion (Guyatt, 1991).
Guyatt himself credits David Sackett—his senior colleague and mentor as one of the strongest influences in shaping the evidence-based movement. Sackett later became the founding chair of the first department of clinical epidemiology and biostatistics at McMaster and played a central role in bringing structure, clarity, and global visibility to EBM.
Shortly after, Scakett and colleagues colleagues formalised the concept. Sackett defined EBM as “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients” (Sackett et al., 1996). This definition highlighted something revolutionary at the time: clinicians must integrate high-quality research with their own expertise while also considering patient values.
As the healthcare landscape evolved, so did the terminology. By the early 2000s, disciplines beyond medicine including physiotherapy, nursing, occupational therapy, and public health emerged. We started to recognise that this approach/concept applied to all health professions. The term Evidence-Based Practice (EBP) gained popularity to reflect this broader, interdisciplinary approach (Straus et al., 2005).
Today, EBP is embedded within professional standards, accreditation guidelines, and clinical decision-making frameworks across health sciences worldwide.
What Exactly Is Evidence-Based Practice?
Evidence-Based Practice expands the original medical model into a more holistic, profession-inclusive approach.
EBP is commonly understood as the integration of:
- Best available research evidence,
- Clinical expertise, and
- Patient values and preferences
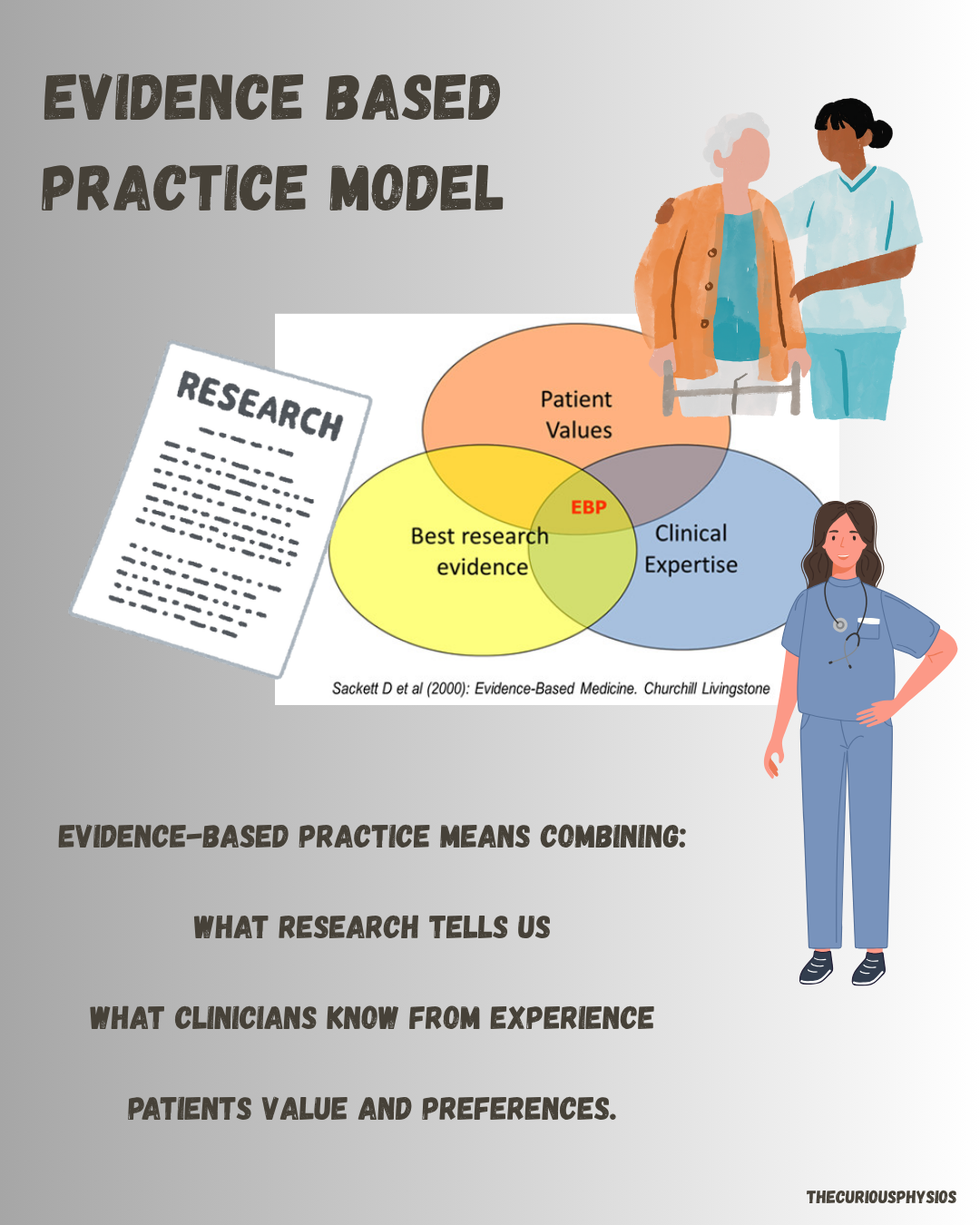
Picture this: A teacher teaches a flashy new technique because there is evidence and he swears it’s “research-based.” Turns out, the “research” was a single unpublished study on 12 patients. Meanwhile, a mountain of rigorous trials sits ignored. EBP is the antidote to that chaos.It forces us to ask three questions before acting:
- What does the research say? (And is it any good?)
- Can I actually apply it here? (Expertise check.)
- Does it fit this person’s life, goals, and beliefs? (Values check.)
When done right, EBP cuts waste, reduces harm, and boosts outcomes. Most texts on EBP informs us of five steps to evidence based practice and these steps forms they way that allows us to base our practice on evidence.
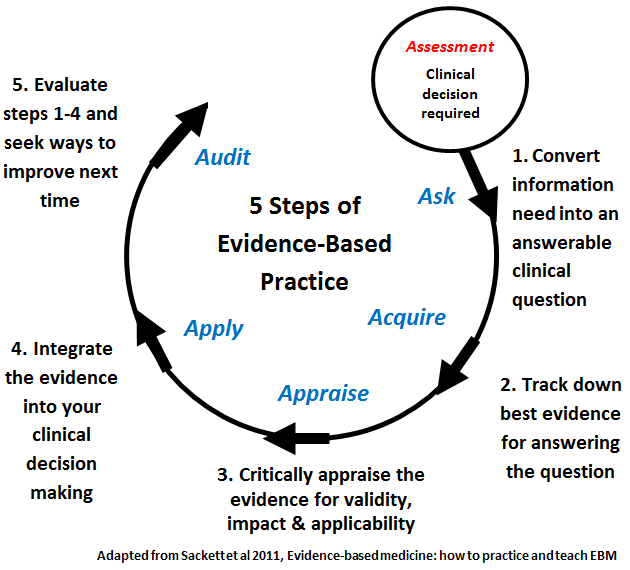
The Five Steps of Evidence-Based Practice
1. Ask a Clinical Question
Everything begins with a well-framed question. Clinicians often use the PICO format to craft focused, answerable questions.
2. Acquire the Evidence
Once the question is clear, the next step is searching for research using reliable databases such as PubMed, PEDro, or Cochrane Library.
3. Appraise the Evidence
This is the critical part—evaluating the quality, validity, and applicability of the evidence. Not all studies carry the same weight, and not all evidence fits every patient.
4. Apply to Practice
Evidence only matters if we use it. This step involves integrating research findings with clinical expertise and patient values to make informed decisions.
5. Assess Outcomes
Finally, we evaluate whether the decision led to the desired outcome. If not, we reflect, refine, and repeat the process.
These five steps keep clinical practice dynamic, accountable, and responsive to new knowledge.
Why EBP Matters in Physiotherapy
In modern physiotherapy, EBP is not optional it is foundational.
It helps clinicians:
- Deliver safer, more effective care
- Avoid outdated or ineffective interventions
- Communicate decisions more clearly with patients
- Contribute to professional growth and lifelong learning
- Strengthen the credibility of the profession in multidisciplinary settings
And importantly, EBP allows patients to become active partners in their care. Involving their values, preferences, and lived experiences creates better engagement and better outcomes.
The Catch (Because There’s Always One)
EBP isn’t a magic wand. Research gaps exist especially in underrepresented populations. Not every question has a randomized trial (try randomizing “parenting styles”). And let’s be honest: reading systematic reviews isn’t exactly beach reading. Plus, evidence can be weaponized. Ever seen a policy maker cherry-pick one study to push an agenda? EBP demands critical appraisal skills, not blind faith.
Remember EBP is not a rigid formula or a checklist to follow blindly. It is a thoughtful, flexible way of working—one that respects science, honours clinical experience, and values the patient’s voice.
From its origins in Evidence-Based Medicine to its widespread adoption across healthcare, EBP continues to shape physiotherapy into a forward-thinking, research-driven, patient-centred profession. As new evidence emerges and our understanding deepens, EBP ensures that our practice evolves with confidence and integrity.
Thanks for Reading!
Ammar Suhail
Leave a comment