Joint sounds; specifically in knee joints have always been a major question asked by the patients. It is often noted when they are asked about their presenting complaints, they do highlight joint crepitus. Patients use various terminologies to describe the sound as ‘grinding’,‘creaking’,‘clunking’. And most of them attribute this to joint “wearing” and “tearing down”. Which is of course questionable.
It’s difficult to define crepitus by both clinicians and patients. Crepitus can be considered as creaking and cracking of joints on movement. It’s a sound produced during movements such as stair climbing, sitting, kneeling, running and many other activities involving knee joints
Recent researches (Robertson, 2010 & 2017; Silva, 2018; Pazinatoo, 2019; Pazinatoo &Silva, 2018) suggest crepitus is not associated with pathological changes or the patient’s presentation. Crepitus is often present in the complete absence of any joint pathology and has no association with functional levels of the patient. So it’s important to make the patient aware of the value of crepitus. In order to do so, we need to understand the underlying people’s beliefs about the meaning of crepitus. Robertson, 2017 explored the patients’ beliefs about crepitus in a qualitative study. Understanding these beliefs will help clinicians address these beliefs and help the patient understand about Knee crepitus.
Let’s have a look at beliefs patients hold about crepitus.
Patients’ “Belief” about crepitus
“Searching for and perceived meaning of noise”
“Something is not right and it makes you worry about the joint“.
“I think it means my knee is wearing away. But I daren’t Google it“.
Patients always want to know what the noise meant. With time rather then getting used to the noise, anxiety develops about what the noise is all about. This needs to be addressed.
Crepitus means you are “ageing”
“It should not be happening at my age…I would equate it more with someone older, say if my mother had noise in her knees and I would be, Oh that is okay, that is older, you know more normal…and so having it at my age is obviously more distressing“
This is what patients deduce out of crepitus and attribute the crepitus to the ageing process. In Robertson paper, many many linked this with their belief that the noise represented bone-on-bone, or wear.
“Too emotional?”
“I am always a little bit scared when I stretch my leg out because I’m thinking, am I going to hear that noise“.
“The crunchiness disturbs me. It makes my skin crawl because it does not sound healthy“.
The patients usually display negative emotions associated with crepitus, which is usually driven by wrong information or no information about the joint sounds.
“Beliefs get influenced by others?”
“My mother will say, ah your knees are not so good..telling me not to kneel down or if I am doing jobs with her like gardening or whatever, she’ll be like, get out of the way, I’ll kneel down’, but she is in her 60’s“
Comments from families and friends served to reinforce negative belief systems. Other than that the noise when experienced in the presence of others they feel self-conscious, and at times embarrassed.
“Professional” answers to their Queries
“Nobody said anything about it even when they asked about the symptoms. I was just completely glossed over and ignored, okay and I suppose maybe it’s because it isn’t important more than the pain to them, but it is to me!“
Robertson highlighted that positive reinforcement by health care providers helped patients and most of the time the explanations helped them get along with noise. But sometimes when this is not addressed it leads to more negative beliefs.
This should be addressed by the attending health care provider to give an explanation to their queries.
“Changing Movements” we do and “Avoiding” Activities in Day-to-Day Life”
“Climbing the stairs and things, I would try and do something a little bit strange with my leg in order to avoid hearing the noise…I was flicking my leg to the side“
“I’m flat hunting at the moment and I’ve decided to only look at ground-floor flats. I’m fed up with the noise. I’m reminded of my knee all the time at work, you know as it’s heavy work. I don’t want to be reminded at home too. It makes me anxious, worried, thinking about it when I don’t want to. I feel a bit silly saying it but that’s the reality“
Patients usually avoid or modify activities which leads to noise. Physical hobbies are affected by participants’ belief about the noise, but for varying reasons.
To summarize it all….!
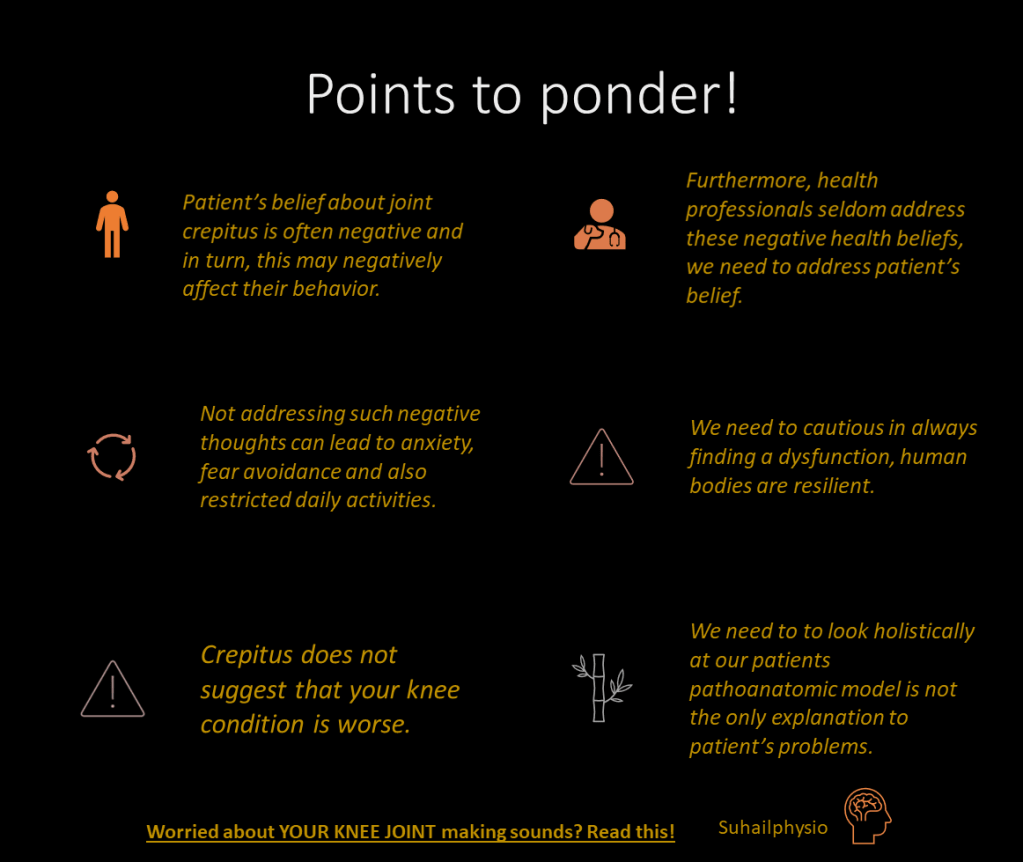
- Crepitus does not suggest that your knee condition is worse
- Patient’s belief about joint crepitus is often negative and in turn, this may negatively affect their behavior.
- Furthermore, health professionals seldom address these negative health beliefs, we need to address the patient’s belief!
- Not addressing such negative thoughts can lead to anxiety, fear avoidance and also restricted daily activities.
- We need to be cautious in always finding a dysfunction, human bodies are resilient.
- We need to look holistically at our patients pathoanatomic model is not the only explanation to patient’s problems.
Enjoy Reading!
References
De Oliveira Silva, D., Barton, C., Crossley, K., Waiteman, M., Taborda, B., Ferreira, A. S., & de Azevedo, F. M. (2018). Implications of knee crepitus to the overall clinical presentation of women with and without patellofemoral pain. Physical Therapy in Sport, 33, 89-95.
De Oliveira Silva, D., Pazzinatto, M. F., Del Priore, L. B., Ferreira, A. S., Briani, R. V., Ferrari, D., … & de Azevedo, F. M. (2018). Knee crepitus is prevalent in women with patellofemoral pain, but is not related with function, physical activity, and pain. Physical Therapy in Sport, 33, 7-11.
Pazzinatto, M. F., de Oliveira Silva, D., Faria, N. C., Simic, M., Ferreira, P. H., de Azevedo, F. M., & Pappas, E. (2019). What are the clinical implications of knee crepitus to individuals with knee osteoarthritis? An observational study with data from the Osteoarthritis Initiative. Brazilian journal of physical therapy, 23(6), 491-496.
Robertson, C. J. (2010). Joint crepitus—are we failing our patients? Physiotherapy Research International, 15(4), 185-188.
Robertson, C. J., Hurley, M., & Jones, F. (2017). People’s beliefs about the meaning of crepitus in patellofemoral pain and the impact of these beliefs on their behaviour: a qualitative study. Musculoskeletal Science and Practice, 28, 59-64.
Ammar Suhail PT
Leave a comment